Catalog Advanced Search
-
Contains 5 Component(s), Includes Credits Includes a Live Web Event on 12/12/2025 at 12:00 PM (CST)
Speaker: Daniel Cerny MUDr., Ph.D.| Immediate adhesive restoration of endodontically treated tooth provides both structural rehabilitation and microbiological isolation to the root canal treated tooth. In the hands of the treating endodontist, it provides both functions on the spot. No insecure period, no risk of reinfection, no need to put rubber dam again. Key elements of such restorations will be provided together with plethora of clinical cases.
CE Hours: 1.0
Description: Immediate adhesive restoration of endodontically treated tooth provides both structural rehabilitation and microbiological isolation to the root canal treated tooth. In the hands of the treating endodontist, it provides both functions on the spot. No insecure period, no risk of reinfection, no need to put rubber dam again. Key elements of such restorations will be provided together with plethora of clinical cases.
Learning Objectives:
- Describe the core principles of root canal treated tooth restoration
- Indicate the limits of adhesive endo-restorations
- Describe appropriate clinical steps and their technical details

Daniel Cerny, MUDr., PhD
Daniel Cerny (*1974) has received his dental degree at the Charles University, Medical School in Hradec Kralove, Czech Republic (1998). Doctorate degree earned at Palacky University in Olomouc in 2018 with the topic of adhesive post-endodontic treatment.
Part-time faculty member at Palacky University Olomouc (2019-2021). Previously an assistant professor at Charles University, Medical School in Hradec Kralove at the Dpt of Conservative Dentistry and Endodontics (1998-2007).
Private practice in Hradec Kralove limited to endodontics and adhesive dentistry since 2001.
Immediate Past President of the Czech Endodontic Association (CES) 2015-2023.Disclosure(s): Micerium: Speaker/Honoraria (includes speakers bureau, symposia, and expert witness) (Ongoing)
-
Contains 5 Component(s), Includes Credits Includes a Live Web Event on 08/27/2025 at 6:00 PM (CDT)
Speaker: Justin Kolnick, DDS|Bacterial testing of root canal systems in patients has traditionally presented with many difficulties. The culture technique never gained wide acceptance as the procedure is arduous and time consuming. DNA-based identification such as polymerase chain reaction suffers from high false positive readings by detecting DNA from dead bacterial cells. A newly introduced ATP assay detection method provides rapid identification of organic residues in root canal systems by detecting ATP, as well as its degradation products ADP and AMP, using a combination of luminescent reactions. The resulting luminescence is measured and displayed as a 0 – 100 Endoscore, with low scores indicating less cellular (bacterial) contamination. The ability to acquire results within 10 seconds can have significant ramifications in endodontics by allowing dentists to assess and modify cleaning and disinfection protocols in real time. Extrapolating data from research in extracted teeth, with artificially created biofilm, to clinical treatment of patients is complicated with potential inaccurate and erroneous inferences. This presentation will review the ATP assay detection method and present data illustrating how this method can be used to validate an Er,Cr:YSGG laser-assisted endodontic protocol for the cleaning and disinfection of root canal systems.
CE Hours: 1.0
Description: Bacterial testing of root canal systems in patients has traditionally presented with many difficulties. The culture technique never gained wide acceptance as the procedure is arduous and time consuming. DNA-based identification such as polymerase chain reaction suffers from high false positive readings by detecting DNA from dead bacterial cells.
A newly introduced ATP assay detection method provides rapid identification of organic residues in root canal systems by detecting ATP, as well as its degradation products ADP and AMP, using a combination of luminescent reactions. The resulting luminescence is measured and displayed as a 0 – 100 Endoscore, with low scores indicating less cellular (bacterial) contamination.
The ability to acquire results within 10 seconds can have significant ramifications in endodontics by allowing dentists to assess and modify cleaning and disinfection protocols in real time. Extrapolating data from research in extracted teeth, with artificially created biofilm, to clinical treatment of patients is complicated with potential inaccurate and erroneous inferences.
This presentation will review the ATP assay detection method and present data illustrating how this method can be used to validate an Er,Cr:YSGG laser-assisted endodontic protocol for the cleaning and disinfection of root canal systems.
Learning Objectives:
- Describe a rapid chair-side test for root canal cleanliness
- Test to evaluate endodontic treatment protocols.
- Describe how this test can be utilized to evaluate the efficacy of a laser-assisted endodontic protocol, utilizing an Er,Cr:YSGG laser, for the cleaning and disinfection of complex root canal systems.

Justin Kolnick, DDS
Dr. Kolnick received his dental degree, cum laude, from the University of the Witwatersrand in South Africa, where he was the first dental school graduate to be awarded the University Scholarship for Overseas Postgraduate Study. He received his postdoctoral endodontic training from Columbia University in the City of New York.
Dr. Kolnick has been committed to endodontic education, first as an Associate Clinical Professor in Endodontics at Columbia University and then as an Attending at Westchester Medical Center and an Associate Clinical Professor in Endodontics at New York Medical College. Although he no longer holds these positions, he continues to lecture extensively on local, national and international levels and has published several articles on endodontics. Dr. Kolnick is dedicated to fostering excellence in endodontics through education and the incorporation of the latest technology. For the past 18 years, his experience and expertise in lasers has made a significant contribution to the development of a comprehensive, laser-assisted treatment concept in endodontics.
Disclosure(s): Biolase, EdgeEndo: Consultant, Honorarium/Gift
-
Contains 5 Component(s), Includes Credits Includes a Live Web Event on 08/05/2025 at 7:00 PM (CDT)
Speaker: Lynn M. Gaumer, J.D., CAP®|Are you a practice owner preparing for transition, selling your practice, or planning for retirement? Or perhaps you’re still in the midst of your career, but want to ensure your personal and charitable wishes are clearly documented. Join us for a one-hour complimentary webinar in celebration of Make a Will Month! This session will cover the essentials of estate planning and how charitable giving can play a pivotal role in your legacy. With new tax laws potentially on the horizon, now is the perfect time to explore tax-saving strategies that benefit you and the causes you care about. Don’t miss the opportunity to ensure your estate and charitable plans are in order and to make a lasting impact. This can be your first step towards leaving a legacy that endures for generations to come.
CE Hours: 1.0
Description: Are you a practice owner preparing for transition, selling your practice, or planning for retirement? Or perhaps you’re still in the midst of your career, but want to ensure your personal and charitable wishes are clearly documented.
Join us for a one-hour complimentary webinar in celebration of Make a Will Month! This session will cover the essentials of estate planning and how charitable giving can play a pivotal role in your legacy. With new tax laws potentially on the horizon, now is the perfect time to explore tax-saving strategies that benefit you and the causes you care about.
Don’t miss the opportunity to ensure your estate and charitable plans are in order and to make a lasting impact. This can be your first step towards leaving a legacy that endures for generations to come.
Learning Objectives:
- Gain a clear overview of basic estate planning principles with relevance to endodontists and dental practice owners, including wills, trusts, and powers of attorney.
- Explore the essential documents and strategic considerations that ensure both personal and practice-related assets are protected and aligned with professional goals.
- Discover the most effective and popular tools — such as bequests, donor-advised funds, and charitable trusts — that dental professionals can use to leave a lasting legacy through philanthropic contributions to causes like oral health, education, or professional foundations.
This webinar is free for AAE members

Lynn M. Gaumer, J.D., CAP®
Lynn M. Gaumer, J.D., CAP® is the senior gift planning consultant for The Stelter Company and a board member of both the Mid-Iowa Planned Giving Council and the National Association of Charitable Gift Planners, where she previously chaired the Leadership Institute. She is also a member of NACGP’s 2025 Development and Government Relations Committees.
With over 25 years of experience in estate and charitable planning, Lynn has spent more than 13 years at Stelter, advising clients on technical planned giving matters and ensuring the accuracy of nonprofit marketing communications. She regularly presents technical webinars for Stelter, speaks at conferences nationwide on a variety of planned giving topics, and authors Stelter’s Expert Insights, a publication covering trends and research in planned giving. Her expertise has also been featured in Planned Giving Today, where she has published two articles.
Before joining Stelter, Lynn spent a decade as an associate attorney specializing in estate and charitable planning.
She earned her B.A. in economics and communication studies from the University of Iowa and her J.D. from the University of South Dakota School of Law.
Lynn has three grown children and resides in Ankeny, Iowa, with her husband, Craig, and their “mystery mutt,” Cosmo.
In accordance with this policy, I declare that I have NO past or present proprietary or relevant, financial relationship or receive gifts in kind (including soft intangible remuneration), consulting position or affiliation, or other personal interest of any nature or kind in any product, service, course and/or company, or in any firm beneficially associated therewith.
-
Contains 5 Component(s), Includes Credits
Authors: Yuhong Lin, DDS, Vivek Thumbigere-Math, BDS, PhD, Anil Kishen, BDS, MDS, PhD, and Jianing He, DMD, PhD|Multiple Cervical Root Resorption (MCRR) is a rare condition characterized by the progressive destruction of the cervical region of multiple tooth roots, leading to significant tooth loss. The etiology and pathogenesis of MCRR remain poorly understood. Existing knowledge is largely derived from case reports/series. A comprehensive review of literature is crucial to identify potential systemic and dental factors that contribute to the development and progression of MCRR.
CE Hours: 1.0
Description: Multiple Cervical Root Resorption (MCRR) is a rare condition characterized by the progressive destruction of the cervical region of multiple tooth roots, leading to significant tooth loss. The etiology and pathogenesis of MCRR remain poorly understood. Existing knowledge is largely derived from case reports/series. A comprehensive review of literature is crucial to identify potential systemic and dental factors that contribute to the development and progression of MCRR.
At the conclusion of this article, the reader will be able to:
- Describe the systemic diseases, genetic mutations, and medications that have been implicated in multiple cervical root resorption.
- Discuss the common pathogenic pathways shared by multiple cervical root resorption and conditions affecting the skeletal system.
- Describe the role of interdisciplinary collaboration in the diagnosis and management of multiple cervical root resorption.

Yuhong Lin, DDS
Dr. Yuhong Lin is a second year Endodontics resident at Texas A&M University College of Dentistry. She received her dental degree from UTHealth Houston School Dentistry.

Vivek Thumbigere-Math, BDS, PhD
Vivek Thumbigere Math, BDS, PhD, is a board-certified periodontist and Assistant Professor in the Division of Periodontics at the University of Maryland School of Dentistry. He is nationally an internationally recognized for his leadership in periodontology, combining excellence in clinical care, education, and translational research to improve oral and systemic health outcomes. Dr. Math earned his Bachelor of Dental Surgery (BDS) in India, followed by a PhD and residency training in Periodontology at the University of Minnesota. He subsequently completed a prestigious postdoctoral fellowship at the National Institutes of Health (NIH) under the mentorship of Dr. Martha Somerman (former director of NIDCR). At the University of Maryland, Dr. Math provides advanced periodontal and implant care with a strong emphasis on evidence-based, patient-centered treatment. As a passionate educator, Dr. Math mentors dental students and periodontology residents while actively contributing to curriculum development and innovation. His research focuses on periodontal disease pathogenesis, osteoimmunology, and the intersection between oral and systemic diseases. His research program has been continuously supported by competitive NIH funding. He has authored over 40 peer-reviewed publications in leading scientific journals and is a frequently invited speaker at national and international conferences. Dr. Math serves on multiple NIH study sections and editorial boards, and is currently Associate Editor of Frontiers in Dental Medicine.

Anil Kishen, B.D.S., M.D.S., Ph.D.
Dr. Anil Kishen is the Dean, Zwingenberger Decanal Chair, and Professor ofEndodontics at the Faculty of Dentistry, University of Toronto. He also holds aTier 1 Canada Research Chair in Oral Health Nanomedicine.
Dr. Kishen has received numerous honors, including the 2020Louis I. Grossman Award from the American Association of Endodontists, the 2023National Dental Research Award (CADR/ACFD), the W. W. Wood Award for excellencein dental education, and the Enterprise Challenge Innovator Award in Singapore.
He has published over 300 journal articles, 24 bookchapters, and three books, and holds 12 patents. He has delivered more than 200invited lectures globally and serves as Associate Editor for several leadingjournals, including the Journal of Endodontics.
His research, funded by federal and foundation grants,focuses on wound healing, nanoparticle-guided tissue engineering, andmicrobe–host cell interactions.

Jianing He, D.M.D., Ph.D.
Dr. Jianing (Jenny) He received her dental degree from West China University of Medical Sciences in 1996, and a certificate in Endodontics and a PhD in Oral Biology from the University of Connecticut Health Center in 2003.
Dr. He has been actively involved in endodontic education, research, and clinical practice. She is a Diplomate of the American Board of Endodontics, and a fellow of American College of Dentists. She has published over 50 manuscripts in peer-reviewed journals and co-authored chapters in 4 textbooks including Pathways of the Pulp. Dr. He served on the Regenerative Endodontics committee, Research and Scientific Affairs committee for the AAE, and she is currently an Associate Editor of the Journal of Endodontics.
Dr. He is an Adjunct Professor at Texas A&M University College of Dentistry, and maintains a full-time private practice limited to Endodontics in McKinney and Flower Mound, Texas.
Speaker Disclosure
In accordance with this policy, I declare I have a past or present proprietary or relevant financial relationship or receive gifts in kind (including soft intangible remuneration), consulting position or affiliation, or other personal interest of any nature or kind in any product, service, course and/or company, or in any firm beneficially associated therewith, as indicated: Brasseler USA (Individual(s) Involved: Self): Honorarium (Terminated)
-
Contains 5 Component(s), Includes Credits
Speaker: Gabriela Lagreca, DMD|We'll examine key survival rates and success metrics for both options, delving into the fundamental distinctions between teeth and implants. The presentation identifies crucial factors that influence tooth preservation and evaluates the documented evidence regarding implant performance over time compared to natural dentition. Drawing from current research, we'll analyze which restoration approaches and treatment strategies demonstrate optimal long-term outcomes. This evidence-based discussion aims to provide clarity on the durability and effectiveness of both treatment pathways, helping inform clinical decision-making for lasting dental solutions.
CE Hours: 1.0
Description:
We'll examine key survival rates and success metrics for both options, delving into the fundamental distinctions between teeth and implants. The presentation identifies crucial factors that influence tooth preservation and evaluates the documented evidence regarding implant performance over time compared to natural dentition. Drawing from current research, we'll analyze which restoration approaches and treatment strategies demonstrate optimal long-term outcomes. This evidence-based discussion aims to provide clarity on the durability and effectiveness of both treatment pathways, helping inform clinical decision-making for lasting dental solutions.
Learning Objectives:
- Explain the similarities and differences between a tooth and an implant in terms of long-term survival
- Recognize the factors for clinically acceptable results and success
- Discuss treatment planning alternatives and sustainability of treatment
Gabriela Lagreca, DDS, DMD, MBA, FACP
Dr. Lagreca is a Board-Certified Prosthodontist and fellow of the American Board of Prosthodontics. She received her first dental degree (DDS) from the Universidad Central de Venezuela in Caracas. She then received her certificate in Prosthodontics, Implant Fellowship training and and currently Doctor of Dental Medicine (DMD) degrees from Tufts University School of Dental Medicine (TUSDM). Dr. Lagreca teaches in classroom, clinical and preclinical prosthodontics to pre and postdoctoral residents and supports the Office of Academic Affairs in faculty development, training, and calibration. Dr. Lagreca is the President of the American College of Prosthodontics Massachusetts section, where she leads the prosthodontics community in the state, organizes continuing education programs and collaborates with dental professionals and educators from Harvard, Tufts and Boston University. Dr. Lagreca’s achievements have been recognized by the Incisal Edge Magazine 40-under-40 2021 Award and The American Dental Association.
In accordance with this policy, I declare I do not have a past or present proprietary or relevant financial relationship or receive gifts in kind (including soft intangible remuneration), consulting position or affiliation, or other personal interest of any nature or kind in any product, service, course and/or company, or in any firm beneficially associated therewith, as indicated.
-
Contains 5 Component(s), Includes Credits
Authors: Tatiana A. M. do Nascimento, MSc, Francielle S. Verner, PhD, Cleidiel Aparecido Araujo Lemos, PhD, and Rafael B. Junqueira, PhD|The aim of this study was to perform a qualitative and quantitative synthesis of the available studies evaluating the possible relationship between apical periodontitis and autoimmune diseases.
CE Hours: 1.0
Description: The aim of this study was to perform a qualitative and quantitative synthesis of the available studies evaluating the possible relationship between apical periodontitis and autoimmune diseases.
At the conclusion of this article, the reader will be able to:
- Describe the possible association between apical periodontitis and autoimmune diseases, based on the evidence presented in the systematic review and meta-analysis.
- Assess the methodological quality of the studies included in the article, identifying limitations, risks of bias and level of certainty of the evidence.
- Discuss the clinical implications of the article's findings for dental practice, especially in the management of patients with autoimmune diseases.

Tatiana A M do Nascimento, DDS
DDS, Specialist (Endodontics and Periodontics), Private Practice. MSc student at Health Applied Sciences Postgraduate Program, Federal University of Juiz de Fora, Campus GV, Governador Valadares, Brazil.

Francielle S Verner, DDS, MSc, PhD
DDS, Specialist (Oral Radiology), MSc (Dental Clinic), PhD (Oral Radiology). Professor at Department of Dentistry, Federal University of Juiz de Fora, Campus GV, Governador Valadares, Brazil.

Cleidiel A A Lemos, DDS, MSc, PhD
DDS, Specialist (Prosthodontics), MSc (Prosthodontics), PhD (Prosthodontics). Professor at Department of Dentistry, Federal University of Juiz de Fora, Campus GV, Governador Valadares, Brazil.
Rafael B Junqueira, DDS, MSc, PhD
DDS, Specialist (Endodontics), MSc (Dental Clinic), PhD (Endodontics). Professor at Department of Dentistry, Federal University of Juiz de Fora, Campus GV, Governador Valadares, Brazil.
-
Contains 5 Component(s), Includes Credits
Speaker: Nelson L. Rhodus, DMD, MPH, FICD, FRCSEd|Systemic health is related to oral health and vice versa. Many systemic diseases are manifested in the oral cavity and many oral conditions and therapies have a profound impact upon systemic diseases. In addition, some of the therapies used to these conditions have significant effects on the oral cavity. For those reasons, it is important for dentists ( and dental health care professionals) to know about their patients' medical conditions before treating them and to understand which diseases manifest themselves in the oral cavity. This course will present a thorough overview of the principles of the management of medical conditions in dental patients, Furthermore, the participant will be updated upon current understanding and treatment of oral conditions such as oral cancer, xerostomia, lichen planus and candidiasis among others.
CE Hours: 1.5
Description: Systemic health is related to oral health and vice versa. Many systemic diseases are manifested in the oral cavity and many oral conditions and therapies have a profound impact upon systemic diseases. In addition, some of the therapies used to these conditions have significant effects on the oral cavity. For those reasons, it is important for dentists ( and dental health care professionals) to know about their patients' medical conditions before treating them and to understand which diseases manifest themselves in the oral cavity. This course will present a thorough overview of the principles of the management of medical conditions in dental patients, Furthermore, the participant will be updated upon current understanding and treatment of oral conditions such as oral cancer, xerostomia, lichen planus and candidiasis among others.
Learning Objectives:
- Describe the changing epidemiology of medical problems in dental patients
- Review the medical manifestations and treatment options for medical problems in dental patients
- Identify the oral manifestations and potential complications of medical problems in dental patients
Educational support provided by Endodontic Practice Partners
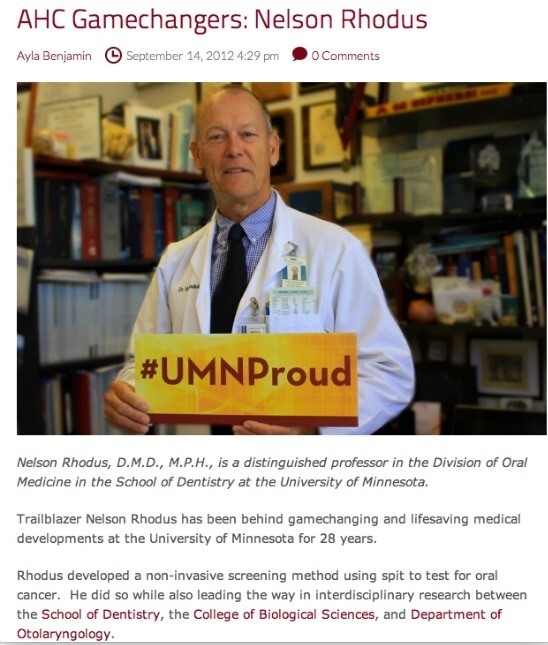
Nelson L. Rhodus, D.M.D., M.P.H.
NELSON L RHODUS, DMD, MPH, FICD, FRCSEd, FAAOM, Diplomate American Board of Oral Medicine, is a Morse Distinguished Professor and Director of the Division of Oral Medicine, Oral Diagnosis and Radiology in the Department of Diagnostic and Biological Sciences in the University of Minnesota School of Dentistry. He is also an Adjunct Professor of Otolaryngology in the Medical School and an Adjunct Professor of Epidemiology in the School of Public Health . He is a Diplomate, examiner and past President of the American Board of Oral Medicine, He is also past President of the American Academy of Oral Medicine. He is an inductee in the University of Minnesota Academic Health Center Academy of Excellence and the Academy of Distinguished Teachers and the University of Minnesota Scholar’s Walk of Fame. He is a Fellow in the International College of Dentists and of the American College of Dentists and a Fellow in the Royal College of Surgeons of Edinburgh. He is an Attending member of the Minnesota Masonic Cancer Center and the Hospital Staff of the University of Minnesota Hospital and Clinics, a consultant to the US Navy Hospital and Hennepin County Medical Center.
Dr. Rhodus directs several oral medicine courses and has been awarded "Professor of the year " for fourteen years and is a recipient the School of Dentistry Century Club Professor of the Year . He has been active in faculty governance and served in many capacities in the University Senate for over 27 years.
Dr. Rhodus has been active with the American Dental Association and the Minnesota Dental Association having served on several committees and the editorial board and has been selected often( x 10) as Best Dentist by Minnesota Monthly and Top Dentist-USA.
Dr. Rhodus has been active in basic and clinical research for over 38 years and he has published over three hundred- eighty refereed scientific papers and abstracts. His H index is 42 and his research has been cited over 5000 times. He has presented over seven-hundred lectures and courses throughout the United States and abroad. He is on the medical advisory board for the National Oral Cancer Foundation and the National Sjogren’s Syndrome Foundation. He is an editor of the Journal of Oral Surgery, Oral medicine, Oral Pathology and Oral Radiology. He co-authors two textbooks: DENTAL MANAGEMENT OF THE MEDICALLY COMPROMISED PATIENT (10ed.) and OROFACIAL DISORDERS.In accordance with this policy, I declare I have a past or present proprietary or relevant financial relationship or receive gifts in kind (including soft intangible remuneration), consulting position or affiliation or other personal interest of any nature or kind in any product service, course, and/or company, or in any firm beneficially associated therewith as indicated below:
Disclosure(s): NIH, SSF (Grants/Research Support), US Army, Navy, VA (Consultant)
-
Contains 5 Component(s), Includes Credits
Authors: Yuxuan Liu, DDS, Yi Luo, DDS, Yaxu Feng, DDS, Xianhua Gao, DDS, Wei Fan, DDS, PhD, and Bing Fan, DDS, MSc, PhD|This study aimed to assess the effect of cavity designs on instrumentation, obturation and fracture resistance for mandibular first premolars with Vertucci V canal.
CE Hours: 1.0
Description: This study aimed to assess the effect of cavity designs on instrumentation, obturation and fracture resistance for mandibular first premolars with Vertucci V canal.
At the conclusion of this article, the reader will be able to:
- Discuss which cavity design is appropriate for mandibular first premolars with Vertucci V canal.
- Compare the effectiveness of different cavity designs in instrumentation, obturation and preservation of dentin and fracture resistance.
- Describe the steps of preparing an access cavity for premolars with Vertucci V canal.

Yuxuan Liu, DDS

Yaxu Feng, DDS

Xianhua Gao, DDS

Wei Fan, DDS, PhD

Bing Fan, DDS, MSc, PhD
-
Contains 5 Component(s), Includes Credits
Speaker: Bettina Basrani, D.D.S., Ph.D., M.Sc.; Ove A. Peters, D.MD, M.S., PhD|Endodontic complications of varying severity can unfortunately occur during most stages of endodontic treatment. This lecture aims to enhance understanding of common endodontic complications and recommends current management and solutions with an evidence-based approach. Preoperative, intraoperative and postoperative issues will be discussed, including possible aetiologies and prevention during root canal therapy. We will address the impact of complications on both patients and practitioners, underscoring the importance of clear communication in preserving the clinician-patient relationship. Attendees will gain current advice and knowledge on how to tackle endodontic complications effectively, fostering excellence in clinical practice and improved patient care.
CE Hours: 1.5
Description: Endodontic complications of varying severity can unfortunately occur during most stages of endodontic treatment. This lecture aims to enhance understanding of common endodontic complications and recommends current management and solutions with an evidence-based approach. Preoperative, intraoperative and postoperative issues will be discussed, including possible aetiologies and prevention during root canal therapy. We will address the impact of complications on both patients and practitioners, underscoring the importance of clear communication in preserving the clinician-patient relationship. Attendees will gain current advice and knowledge on how to tackle endodontic complications effectively, fostering excellence in clinical practice and improved patient care.
Learning Objectives:
- Recognize and identify common endodontic complications.
- Implement evidence based management strategies.
- Develop strategies for preventing endodontic complications.

Bettina R. Basrani D.D.S., M.S.D., Ph.D.
Dr. Bettina Basrani is Tenured Associate Professor and Director, MSc Program in Endodontics at the Faculty of Dentistry, University of Toronto, Ontario, Canada since 2015. Dr Basrani received her DDS degree from the University of Buenos Aires and a Specialty Diploma in Endodontics and PhD from Maimonides University in Buenos Aires, Argentina. A long-time educator and researcher, she began her teaching career at the University of Buenos Aires. In 2000, she moved to Canada to serve as Chair of the Endodontic Program at Dalhousie University, Halifax, Nova Scotia. In 2004, she moved to Toronto, where she has continued her academic and clinical work. Internationally recognized as a leading authority in endodontics and as an excellent lecturer, effectively combining clinical and scientific information, Dr Basrani has received many awards throughout her career, such as the Louis Grossman Award by the French Society of Endodontics and has international courses and lectures, over 40 peer-reviewed scientific publications, three textbooks and several textbook chapters, and abstracts to her credit.
Speaker Disclosure
In accordance with this policy, I declare that I have NO past or present proprietary or relevant financial relationship or receive gifts in kind (including soft intangible remuneration), consulting position or affiliation, or other personal interest of any nature or kind in any product, service, course and/or company, or in any firm beneficially associated therewith.

Ove A. Peters, D.M.D., Ph.D., M.Sc.
Dr. Ove A. Peters joined the University of Queensland, Brisbane, Australia, in 2020 after faculty positions in Heidelberg, Germany and Zurich, Switzerland, as well as at the University of California, San Francisco. He currently serves as the Professor of Endodontics and Head of Clinical Dentistry at UQ. Before moving to Australia, Dr. Peters was the founding director of the postgraduate endodontic program at the Arthur A. Dugoni School of Dentistry in San Francisco, a professor with tenure and the Chair of the Department of Endodontics at that school.
Dr. Peters has wide-ranging clinical and research expertise and has published more than 230 manuscripts related to endodontic technology and biology. He has authored two books and contributed to several leading textbooks in dentistry; he also is an associate editor for the International Endodontic Journal as well as the Australian Endodontic Journal, an academic editor for PLOS One and serves on the review panel of multiple other journals. Among others awards, Dr Peters has received the Hans Genet Award of the European Society of Endodontology and more recently the Louis I. Grossman Award of the American Association of Endodontists. He is a Diplomate of the ABE, a member of OKU and a Fellow of the International and American Colleges of Dentistry.Disclosure(s): Dentsply Sirona: Grant/Research Support (Ongoing), Honorarium (Ongoing), Speaker/Honoraria (includes speakers bureau, symposia, and expert witness) (Ongoing)
-
Contains 5 Component(s), Includes Credits
Speaker: Xiaofei Zhu, DDS, CAGS|Numerous studies indicate the clinical success of regenerative endodontic procedures (REPs), as evidenced by symptom resolution, apical closure, canal wall thickening and lengthening, and restored reaction to vitality tests. However, the true nature of the regenerated human tissue after REPs remains unclear. Animal studies, employing various experimental protocols, have reported the greatest prevalence formation of cementum-like tissue, followed by bone-like tissue, and, to a lesser extent, dentin-like tissue. The question arises: does this conclusion also hold true for patients undergoing REPs? Ethical considerations preclude the conduct of cohort studies or randomized controlled trials in humans to evaluate histological outcomes of REPs. Nonetheless, a limited subset of investigations has delved into the histological outcomes after REPs, offering insights into the regenerative processes involved.Our case-report-based systematic review, encompassing studies from PubMed, Embase, and Web of Science, yielded 17 articles reporting on 22 teeth (mature and immature) from a total of 389 studies published between 2001 and 2023. The findings indicate a predominant presence of fibrous connective tissue, along with cementum-like, and bone-like tissues, whereas true dentinal regeneration is notably rare. Histological outcomes may vary based on factors such as the preoperative condition of the tooth, disinfection protocols, and procedural techniques. Furthermore, through a series of REPs cases from the presenter, we we’re going to discuss potential predictive factors influencing outcomes, including the status of the apical papilla, residual pulp tissue, patient age, and others.
CE Hours: 0.75
Description: Numerous studies indicate the clinical success of regenerative endodontic procedures (REPs), as evidenced by symptom resolution, apical closure, canal wall thickening and lengthening, and restored reaction to vitality tests. However, the true nature of the regenerated human tissue after REPs remains unclear. Animal studies, employing various experimental protocols, have reported the greatest prevalence formation of cementum-like tissue, followed by bone-like tissue, and, to a lesser extent, dentin-like tissue. The question arises: does this conclusion also hold true for patients undergoing REPs? Ethical considerations preclude the conduct of cohort studies or randomized controlled trials in humans to evaluate histological outcomes of REPs. Nonetheless, a limited subset of investigations has delved into the histological outcomes after REPs, offering insights into the regenerative processes involved.Our case-report-based systematic review, encompassing studies from PubMed, Embase, and Web of Science, yielded 17 articles reporting on 22 teeth (mature and immature) from a total of 389 studies published between 2001 and 2023. The findings indicate a predominant presence of fibrous connective tissue, along with cementum-like, and bone-like tissues, whereas true dentinal regeneration is notably rare. Histological outcomes may vary based on factors such as the preoperative condition of the tooth, disinfection protocols, and procedural techniques. Furthermore, through a series of REPs cases from the presenter, we we’re going to discuss potential predictive factors influencing outcomes, including the status of the apical papilla, residual pulp tissue, patient age, and others.
Learning Objectives:
- List the histological findings after REPs in animal study and human case reports.
- Discuss potential predictive factors influencing REPs outcomes.
- Perform REPs more confidently on selected cases.

Xiaofei Zhu, D.M.D
Dr. Xiaofei Zhu is an Assistant Professor and the Director of Research in the Endodontics Department at Boston University School of Dental Medicine. He received his DDS from Peking University, Beijing, China, in 2009. Since then, he had worked as an assistant professor and later as an associate professor (in 2015) at his alma mater. Dr. Zhu joined the Boston University Postgraduate Endodontic Program in 2019. He served on the Regenerative Endodontics committee of the AAE from 2020 to 2021. In 2021, Dr. Zhu started working at Boston University. He earned the Diplomate of the American Board of Endodontics in 2022. Dr. Zhu's primary research interest relates to dental pulp regeneration and stem cells.
Speaker Disclosure
I declare that I have no proprietary, financial, or other personal interest of any nature or kind in any product, service, course, and/or company, or in any firm beneficially associated therewith, that will be discussed or considered during the proposed presentation.

