Catalog Advanced Search
-
Contains 5 Component(s), Includes Credits Includes a Live Web Event on 12/12/2025 at 12:00 PM (CST)
Speaker: Daniel Cerny MUDr., Ph.D.| Immediate adhesive restoration of endodontically treated tooth provides both structural rehabilitation and microbiological isolation to the root canal treated tooth. In the hands of the treating endodontist, it provides both functions on the spot. No insecure period, no risk of reinfection, no need to put rubber dam again. Key elements of such restorations will be provided together with plethora of clinical cases.
CE Hours: 1.0
Description: Immediate adhesive restoration of endodontically treated tooth provides both structural rehabilitation and microbiological isolation to the root canal treated tooth. In the hands of the treating endodontist, it provides both functions on the spot. No insecure period, no risk of reinfection, no need to put rubber dam again. Key elements of such restorations will be provided together with plethora of clinical cases.
Learning Objectives:
- Describe the core principles of root canal treated tooth restoration
- Indicate the limits of adhesive endo-restorations
- Describe appropriate clinical steps and their technical details

Daniel Cerny, MUDr., PhD
Daniel Cerny (*1974) has received his dental degree at the Charles University, Medical School in Hradec Kralove, Czech Republic (1998). Doctorate degree earned at Palacky University in Olomouc in 2018 with the topic of adhesive post-endodontic treatment.
Part-time faculty member at Palacky University Olomouc (2019-2021). Previously an assistant professor at Charles University, Medical School in Hradec Kralove at the Dpt of Conservative Dentistry and Endodontics (1998-2007).
Private practice in Hradec Kralove limited to endodontics and adhesive dentistry since 2001.
Immediate Past President of the Czech Endodontic Association (CES) 2015-2023.
Co-founder and the first president of Czech Academy of Dental Esthetics (CADE) (2007-2009).
Editorial board member of LKS journal (Czech Dental Chamber Journal) (2009-2013)
Co-owner and CEO of the continuing education institute HDVI since 2010. Co-founder of the Dental Summit Congress in Prague (Since 2011).
Author/co-author of 35 articles in dental journals. Co-author of 4 chapters in dental books. Lectures widely internationally.Disclosure(s): Honorarium/Gift: Micerium SpA; Financial/Material Support: Micerium SpA
-
Contains 5 Component(s), Includes Credits Includes a Live Web Event on 08/27/2025 at 6:00 PM (CDT)
Speaker: Justin Klonick, DDS|Bacterial testing of root canal systems in patients has traditionally presented with many difficulties. The culture technique never gained wide acceptance as the procedure is arduous and time consuming. DNA-based identification such as polymerase chain reaction suffers from high false positive readings by detecting DNA from dead bacterial cells. A newly introduced ATP assay detection method provides rapid identification of organic residues in root canal systems by detecting ATP, as well as its degradation products ADP and AMP, using a combination of luminescent reactions. The resulting luminescence is measured and displayed as a 0 – 100 Endoscore, with low scores indicating less cellular (bacterial) contamination. The ability to acquire results within 10 seconds can have significant ramifications in endodontics by allowing dentists to assess and modify cleaning and disinfection protocols in real time. Extrapolating data from research in extracted teeth, with artificially created biofilm, to clinical treatment of patients is complicated with potential inaccurate and erroneous inferences. This presentation will review the ATP assay detection method and present data illustrating how this method can be used to validate an Er,Cr:YSGG laser-assisted endodontic protocol for the cleaning and disinfection of root canal systems.
CE Hours: 1.0
Description: Bacterial testing of root canal systems in patients has traditionally presented with many difficulties. The culture technique never gained wide acceptance as the procedure is arduous and time consuming. DNA-based identification such as polymerase chain reaction suffers from high false positive readings by detecting DNA from dead bacterial cells.
A newly introduced ATP assay detection method provides rapid identification of organic residues in root canal systems by detecting ATP, as well as its degradation products ADP and AMP, using a combination of luminescent reactions. The resulting luminescence is measured and displayed as a 0 – 100 Endoscore, with low scores indicating less cellular (bacterial) contamination.
The ability to acquire results within 10 seconds can have significant ramifications in endodontics by allowing dentists to assess and modify cleaning and disinfection protocols in real time. Extrapolating data from research in extracted teeth, with artificially created biofilm, to clinical treatment of patients is complicated with potential inaccurate and erroneous inferences.
This presentation will review the ATP assay detection method and present data illustrating how this method can be used to validate an Er,Cr:YSGG laser-assisted endodontic protocol for the cleaning and disinfection of root canal systems.
Learning Objectives:
- Describe a rapid chair-side test for root canal cleanliness
- Test to evaluate endodontic treatment protocols.
- Describe how this test can be utilized to evaluate the efficacy of a laser-assisted endodontic protocol, utilizing an Er,Cr:YSGG laser, for the cleaning and disinfection of complex root canal systems.

Justin Klonick, DDS
Dr. Kolnick received his dental degree, cum laude, from the University of the Witwatersrand in South Africa, where he was the first dental school graduate to be awarded the University Scholarship for Overseas Postgraduate Study. He received his postdoctoral endodontic training from Columbia University in the City of New York.
Dr. Kolnick has been committed to endodontic education, first as an Associate Clinical Professor in Endodontics at Columbia University and then as an Attending at Westchester Medical Center and an Associate Clinical Professor in Endodontics at New York Medical College. Although he no longer holds these positions, he continues to lecture extensively on local, national and international levels and has published several articles on endodontics. Dr. Kolnick is dedicated to fostering excellence in endodontics through education and the incorporation of the latest technology. For the past 18 years, his experience and expertise in lasers has made a significant contribution to the development of a comprehensive, laser-assisted treatment concept in endodontics.
Disclosure(s): Biolase, EdgeEndo: Consultant, Honorarium/Gift
-
Contains 5 Component(s), Includes Credits Includes a Live Web Event on 05/21/2025 at 6:00 PM (CDT)
Speaker: Gabriela Lagreca, DMD|We'll examine key survival rates and success metrics for both options, delving into the fundamental distinctions between teeth and implants. The presentation identifies crucial factors that influence tooth preservation and evaluates the documented evidence regarding implant performance over time compared to natural dentition. Drawing from current research, we'll analyze which restoration approaches and treatment strategies demonstrate optimal long-term outcomes. This evidence-based discussion aims to provide clarity on the durability and effectiveness of both treatment pathways, helping inform clinical decision-making for lasting dental solutions.
CE Hours: 1.0
Description:
We'll examine key survival rates and success metrics for both options, delving into the fundamental distinctions between teeth and implants. The presentation identifies crucial factors that influence tooth preservation and evaluates the documented evidence regarding implant performance over time compared to natural dentition. Drawing from current research, we'll analyze which restoration approaches and treatment strategies demonstrate optimal long-term outcomes. This evidence-based discussion aims to provide clarity on the durability and effectiveness of both treatment pathways, helping inform clinical decision-making for lasting dental solutions.
Learning Objectives:
- Explain the similarities and differences between a tooth and an implant in terms of long-term survival
- Recognize the factors for clinically acceptable results and success
- Discuss treatment planning alternatives and sustainability of treatment
Gabriela Lagreca, DDS, DMD, MBA, FACP
Dr. Lagreca is a Board-Certified Prosthodontist and fellow of the American Board of Prosthodontics. She received her first dental degree (DDS) from the Universidad Central de Venezuela in Caracas. She then received her certificate in Prosthodontics, Implant Fellowship training and and currently Doctor of Dental Medicine (DMD) degrees from Tufts University School of Dental Medicine (TUSDM). Dr. Lagreca teaches in classroom, clinical and preclinical prosthodontics to pre and postdoctoral residents and supports the Office of Academic Affairs in faculty development, training, and calibration. Dr. Lagreca is the President of the American College of Prosthodontics Massachusetts section, where she leads the prosthodontics community in the state, organizes continuing education programs and collaborates with dental professionals and educators from Harvard, Tufts and Boston University. Dr. Lagreca’s achievements have been recognized by the Incisal Edge Magazine 40-under-40 2021 Award and The American Dental Association.
In accordance with this policy, I declare I do not have a past or present proprietary or relevant financial relationship or receive gifts in kind (including soft intangible remuneration), consulting position or affiliation, or other personal interest of any nature or kind in any product, service, course and/or company, or in any firm beneficially associated therewith, as indicated.
-
Contains 5 Component(s), Includes Credits Includes a Live Web Event on 04/23/2025 at 6:00 PM (CDT)
Speaker: Nelson L. Rhodus, DMD, MPH, FICD, FRCSEd|Systemic health is related to oral health and vice versa. Many systemic diseases are manifested in the oral cavity and many oral conditions and therapies have a profound impact upon systemic diseases. In addition, some of the therapies used to these conditions have significant effects on the oral cavity. For those reasons, it is important for dentists ( and dental health care professionals) to know about their patients' medical conditions before treating them and to understand which diseases manifest themselves in the oral cavity. This course will present a thorough overview of the principles of the management of medical conditions in dental patients, Furthermore, the participant will be updated upon current understanding and treatment of oral conditions such as oral cancer, xerostomia, lichen planus and candidiasis among others.
CE Hours: 1.5
Description: Systemic health is related to oral health and vice versa. Many systemic diseases are manifested in the oral cavity and many oral conditions and therapies have a profound impact upon systemic diseases. In addition, some of the therapies used to these conditions have significant effects on the oral cavity. For those reasons, it is important for dentists ( and dental health care professionals) to know about their patients' medical conditions before treating them and to understand which diseases manifest themselves in the oral cavity. This course will present a thorough overview of the principles of the management of medical conditions in dental patients, Furthermore, the participant will be updated upon current understanding and treatment of oral conditions such as oral cancer, xerostomia, lichen planus and candidiasis among others.
Learning Objectives:
- Describe the changing epidemiology of medical problems in dental patients
- Review the medical manifestations and treatment options for medical problems in dental patients
- Identify the oral manifestations and potential complications of medical problems in dental patients
Educational support provided by Endodontic Practice Partners
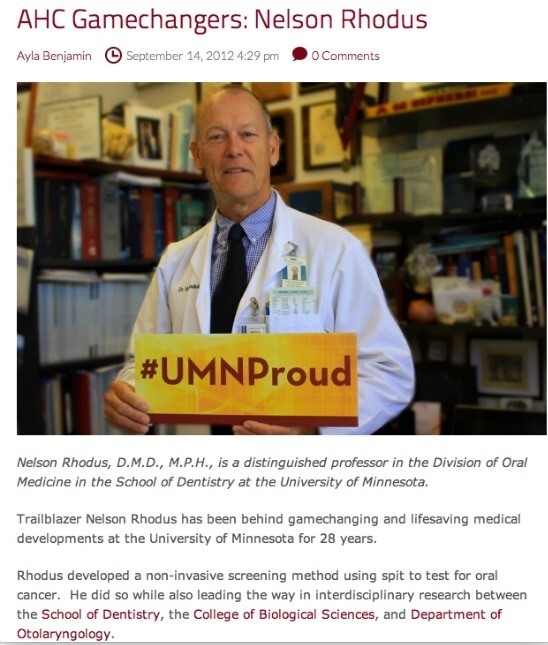
Nelson L. Rhodus, D.M.D., M.P.H.
NELSON L RHODUS, DMD, MPH, FICD, FRCSEd, FAAOM, Diplomate American Board of Oral Medicine, is a Morse Distinguished Professor and Director of the Division of Oral Medicine, Oral Diagnosis and Radiology in the Department of Diagnostic and Biological Sciences in the University of Minnesota School of Dentistry. He is also an Adjunct Professor of Otolaryngology in the Medical School and an Adjunct Professor of Epidemiology in the School of Public Health . He is a Diplomate, examiner and past President of the American Board of Oral Medicine, He is also past President of the American Academy of Oral Medicine. He is an inductee in the University of Minnesota Academic Health Center Academy of Excellence and the Academy of Distinguished Teachers and the University of Minnesota Scholar’s Walk of Fame. He is a Fellow in the International College of Dentists and of the American College of Dentists and a Fellow in the Royal College of Surgeons of Edinburgh. He is an Attending member of the Minnesota Masonic Cancer Center and the Hospital Staff of the University of Minnesota Hospital and Clinics, a consultant to the US Navy Hospital and Hennepin County Medical Center.
Dr. Rhodus directs several oral medicine courses and has been awarded "Professor of the year " for fourteen years and is a recipient the School of Dentistry Century Club Professor of the Year . He has been active in faculty governance and served in many capacities in the University Senate for over 27 years.
Dr. Rhodus has been active with the American Dental Association and the Minnesota Dental Association having served on several committees and the editorial board and has been selected often( x 10) as Best Dentist by Minnesota Monthly and Top Dentist-USA.
Dr. Rhodus has been active in basic and clinical research for over 38 years and he has published over three hundred- eighty refereed scientific papers and abstracts. His H index is 42 and his research has been cited over 5000 times. He has presented over seven-hundred lectures and courses throughout the United States and abroad. He is on the medical advisory board for the National Oral Cancer Foundation and the National Sjogren’s Syndrome Foundation. He is an editor of the Journal of Oral Surgery, Oral medicine, Oral Pathology and Oral Radiology. He co-authors two textbooks: DENTAL MANAGEMENT OF THE MEDICALLY COMPROMISED PATIENT (10ed.) and OROFACIAL DISORDERS.In accordance with this policy, I declare I have a past or present proprietary or relevant financial relationship or receive gifts in kind (including soft intangible remuneration), consulting position or affiliation or other personal interest of any nature or kind in any product service, course, and/or company, or in any firm beneficially associated therewith as indicated below:
Disclosure(s): NIH, SSF (Grants/Research Support), US Army, Navy, VA (Consultant)
-
Contains 5 Component(s), Includes Credits
Speaker: Albert Goerig, D.D.S., M.S.|This program will address the key office systems and business elements needed to move the office to the next level in practice success and enjoyment. Eighty percent of the success and profitability of an endodontic practice is due to the systems and well trained and empowered team that allows the doctor to focus 95% of their time on treatment and patient care. When these systems are implemented office drama and stress is reduced, profitability can double even when the doctor works less days.
CE Hours: 1.0
Description: This program will address the key office systems and business elements needed to move the office to the next level in practice success and enjoyment. Eighty percent of the success and profitability of an endodontic practice is due to the systems and well trained and empowered team that allows the doctor to focus 95% of their time on treatment and patient care. When these systems are implemented office drama and stress is reduced, profitability can double even when the doctor works less days.
Learning Objectives:
- Identify and understand the five key systems that increase office productivity and efficiency. Once these simple autopilot systems are in place, the office runs effortlessly.
- Create and develop the ideal patient schedule that reduces stress and increases office profitability while reducing no-shows and cancellations.
- Develop an effective marketing system that provides you with high-quality patients needed to meet your practice goals.
Albert C. Goerig, D.D.S., M.S.
Dr. Albert “Ace” Goerig graduated from Case Western Reserve University Dental School in 1971. He retired from the Army Dental Corps in 1991 and has been in private practice for 33 years in Olympia, Washington. He is a diplomat of the American Board of endodontics and has written numerous scientific articles on endodontics and has contributed to 3 endodontic textbooks. He co-founded Endo Mastery, a coaching program for endodontists in 1996. Through his practice management seminars and personal coaching, he has worked with over 22% of all endodontists and their teams in the United States and Canada. He continues to see patients 2 days a week in a fun, profitable and effortless practice.
Disclosure(s): Endo Mastery: Ownership Interest (stocks, stock options, patent or other intellectual property or other ownership interest excluding diversified mutual funds) (Ongoing)
-
Contains 5 Component(s), Includes Credits
Authors: Farzaneh Afkhami, DDS, MSc; Sholeh Ghabraei, DDS, MSc; Nasim Hashemi, DDS, MSc; and Ove A. Peters, DMD, MS, PhD|Fear of dentistry, often due to past painful experiences, is a significant barrier preventing patients from visiting dentists. Achieving effective pain control, especially during root canal treatments, is crucial. However, inferior alveolar nerve blocks (IANBs) have a low success rate, influenced by factors such as anxiety, anatomical variations, and technique limitations, leading to anesthesia failure. Although numerous studies have examined the cold test and electric pulp test (EPT) in assessing the success of local anesthesia, no standardized method has been established. This study evaluated the effectiveness of EPT and cold tests in assessing the depth of anesthesia in patients with symptomatic irreversible pulpitis in the mandibular first molar teeth.
CE Hours: 1.0
Description: Fear of dentistry, often due to past painful experiences, is a significant barrier preventing patients from visiting dentists. Achieving effective pain control, especially during root canal treatments, is crucial. However, inferior alveolar nerve blocks (IANBs) have a low success rate, influenced by factors such as anxiety, anatomical variations, and technique limitations, leading to anesthesia failure. Although numerous studies have examined the cold test and electric pulp test (EPT) in assessing the success of local anesthesia, no standardized method has been established. This study evaluated the effectiveness of EPT and cold tests in assessing the depth of anesthesia in patients with symptomatic irreversible pulpitis in the mandibular first molar teeth.
At the conclusion of this article, the reader will be able to:
- Describe the effectiveness of cold and electric pulp tests (EPT) in assessing the success of inferior alveolar nerve blocks (IANB) in patients with symptomatic irreversible pulpitis.
- Evaluate the sensitivity, specificity, and predictive values of the cold test and EPT in diagnosing pulpal anesthesia failure.
- Discuss the clinical implications of combining cold and electric pulp tests for improving diagnostic accuracy in determining pulpal anesthesia success.

Farzaneh Afkhami, DDS, MSc
Dr. Farzaneh Afkhami is a board-certified endodontist and an associate professor at the Department of Endodontics, Tehran University of Medical Sciences, Iran, and holds an academic affiliation with the School of Dentistry, The University of Queensland, Australia. She has authored over 50 research papers related to endodontics in prestigious peer-reviewed journals. Her work has garnered over 1.3 K citations and an h-index of 19 on Google Scholar. Dr. Afkhami has shared her findings at international scientific conferences and has supervised both
undergraduate and postgraduate students. Additionally, she holds a patent on a nanomaterial product as a root canal medicament, further advancing the field of endodontics.

Sholeh Ghabraei, DDS, MSc
Dr Sholeh Ghabraei is board-certified specialist in endodontics. She currently serves as associate professor in endodontics department, Dental school, Tehran university of medical sciences. Her research focuses on various aspects of endodontics including randomized controlled trials of anesthesia and pain control. She published 44 peer reviewed manuscripts.

Nasim Hashemi, DDS, MSc
Dr. Nasim Hashemi is a board-certified specialist in Endodontics. She achieved 2nd rank in the Iranian Endodontic Board Examination in 2025. Her research focuses on various aspects of endodontics including randomized controlled trials of anesthesia and pain control and broken instrument removal.
She has published nine peer-reviewed manuscripts, contributing to advancements in endodontic science.

Ove A. Peters, D.M.D., Ph.D., M.Sc.
Dr. Ove A. Peters joined the University of Queensland, Brisbane, Australia, in 2020 after faculty positions in Heidelberg, Germany and Zurich, Switzerland, as well as at the University of California, San Francisco. He currently serves as the Professor of Endodontics and Head of Clinical Dentistry at UQ. Before moving to Australia, Dr. Peters was the founding director of the postgraduate endodontic program at the Arthur A. Dugoni School of Dentistry in San Francisco, a professor with tenure and the Chair of the Department of Endodontics at that school.
Dr. Peters has wide-ranging clinical and research expertise and has published more than 230 manuscripts related to endodontic technology and biology. He has authored two books and contributed to several leading textbooks in dentistry; he also is an associate editor for the International Endodontic Journal as well as the Australian Endodontic Journal, an academic editor for PLOS One and serves on the review panel of multiple other journals. Among others awards, Dr Peters has received the Hans Genet Award of the European Society of Endodontology and more recently the Louis I. Grossman Award of the American Association of Endodontists. He is a Diplomate of the ABE, a member of OKU and a Fellow of the International and American Colleges of Dentistry.
Disclosure(s): Dentsply Sirona: Grant/Research Support (Ongoing), Speaker/Honoraria (includes speakers bureau, symposia, and expert witness) (Ongoing)
-
Contains 5 Component(s), Includes Credits Recorded On: 12/11/2024
Speaker: George Bruder, D.M.D.|The decision to treat or extract a tooth in the esthetic zone is one of the more complex decisions that a practitioner must make. It is a test of the team’s knowledge and ability to reach the ultimate goal of an esthetic and functional restoration that will last for years to come. All this must be done with the patient’s emotional and financial status considered. This session will focus on the latest challenges in diagnosing endodontically treated teeth that may require surgery to assist in dental dam isolation, apical surgery and/or intentional replantation. This will be both a “why to” presentation focusing on the decision-making process and a “how to” presentation.
CE Hours: 1.0
Description: The decision to treat or extract a tooth in the esthetic zone is one of the more complex decisions that a practitioner must make. It is a test of the team’s knowledge and ability to reach the ultimate goal of an esthetic and functional restoration that will last for years to come. All this must be done with the patient’s emotional and financial status considered. This session will focus on the latest challenges in diagnosing endodontically treated teeth that may require surgery to assist in dental dam isolation, apical surgery and/or intentional replantation. This will be both a “why to” presentation focusing on the decision-making process and a “how to” presentation.
Learning Objectives:
- Obtain a 3D diagnostic database for successful endodontic treatment planning and case acceptance.
- Review Digital Transformation and how we collaborate through new encrypted data opportunities.
- Identify the benefits of collaborative studies

George A. Bruder, D.M.D.
Dr. Bruder was the founding Chair: Department of Endodontics and Director of the Advanced Specialty Education Program in Endodontics at Stony Brook University School of Dental Medicine from 2006 – 2015. In 2012, Dr. Bruder was awarded the prestigious Edward M. Osetek Educator Award from the American Association of Endodontists and is also a member of Omicron Kappa Upsilon, National Dental Honor Society. He is a Diplomate of the American Board of Endodontics and Fellow of the International College of Dentists. Dr. Bruder serves as CEO/President of TruEndo INC and coinvented both TruShape and TruNatomy Endodontic Instruments with Dr. Ove Peters.
Speaker Disclosure
In accordance with this policy, I declare I have a past or present proprietary or relevant financial relationship or receive gifts in kind (including soft intangible remuneration), consulting position or affiliation, or other personal interest of any nature or kind in any product, service, course and/or company, or in any firm beneficially associated therewith, as indicated: Consultant, Dentsply Sirona; CEO/President, TruENdo INC
-
Contains 5 Component(s), Includes Credits
Authors: Mohammad A. Sabeti, DDS, MA, and Heather Kim, DDS|The aim of this systematic review was to evaluate the pooled estimate and relative risk of periapical lesions in natural teeth adjacent to implants.
CE Hours: 1.0
Description: The aim of this systematic review was to evaluate the pooled estimate and relative risk of periapical lesions in natural teeth adjacent to implants.
At the conclusion of this article, the reader will be able to:
- Evaluate the impact of dental implants on the periapical health of adjacent natural teeth.
- Describe the relative risk of developing periapical radiolucent lesions (PARLs) in natural teeth adjacent to implants compared to those adjacent to non-implants.
- Discuss potential mechanisms that may contribute to the development of PARLs in adjacent natural teeth.

Mike Sabeti, DDS, MA
Professor Sabeti received his DDS degree from the University of Texas, Dental Branch at Houston. He completed a program in Periodontics at Tufts School of dental medicine. He served at the postgraduate department of periodontology at the University of Texas, Dental Branch at Houston. He completed a program in Endodontics at Herman Ostrow School of Dentistry of USC. He currently serves as a site visitor on the Commission on Dental Accreditation (CODA). He has been the president of the Northern California Academy of Endodontics. He served as ADEA PASS (ADEA Postdoctoral Application Support Service) for three years. He has been the chair of the Postgraduate Education Curriculum Committee (PECC) at the University of California at San Francisco. He currently serves as Director of postgraduate endodontics at the University of California at San Francisco. He is board-certified. He has made many invited presentations and published along with several textbook chapters and textbooks. In addition, he has received a Certificate in Recognition of Outstanding Services as a Faculty Member for the enhancement of education and clinical excellence, presented by the Advance Endodontics Herman Ostrow School of Dentistry of the University of Southern California, and a Certificate of Appreciation for the Service and Significant Contribution to Periodontal Division, University of Texas. Dental Branch. He was honored by the Haile T. Debas Academy of Medical Educators at the University of California San Francisco with an Excellence in Teaching award.
Speaker Disclosure
I declare that I have no proprietary, financial, or other personal interest of any nature or kind in any product, service, course, and/or company, or in any firm beneficially associated therewith, that will be discussed or considered during the proposed presentation.

Heather Kim, DDS
Heather was born in Seoul, South Korea and raised in New Jersey. She received her Bachelor of Science in Biology from the University of Pennsylvania. Afterwards, she attended dental school at Columbia University and completed a General Practice Residency at Woodhull Hospital in Brooklyn, NY. She is excited to continue her dental training at UCSF.
-
Contains 5 Component(s), Includes Credits
Speaker: Jeffrey J. Tonner, J.D.|Jeff Tonner, a full-time dental malpractice defense attorney, will explore an endodontist's #1 malpractice risk (that can exceed your insurance limits); the four types of patient complaints; the profile of a typical dental malpractice patient; how to chart short fills, over fills, broken files; refunding fees; legal releases; patient termination; and, related topics.
CE Hours: 1.75
Description: Jeff Tonner, a full-time dental malpractice defense attorney, will explore an endodontist's #1 malpractice risk (that can exceed your insurance limits); the four types of patient complaints; the profile of a typical dental malpractice patient; how to chart short fills, over fills, broken files; refunding fees; legal releases; patient termination; and, related topics.
Learning Objectives:
- Identify and understand that #1 dental malpractice risk for endodontists.
- Appreciate that endodontists will experience 2 to 5 dental-legal entanglements in a career.
- Know how to chart the three critical facts when unfortunate events (overfill, shortfill, broken file) occur.

Jeffrey Tonner, J.D.
Dental Malpractice Defense Attorney
Jeffrey J. Tonner, LLC
Jeff Tonner is a full-time dental-malpractice defense attorney in Phoenix, AZ.
Jeff has defended over 4,000 dentists before the dental board and hundreds of dental malpractice cases in superior court. He drafts and regularly reviews dental contracts, including office leases, asset purchase agreement and both employee and independent contractor agreements.
He has written two books for dentists: "Malpractice: What They Don’t Teach You In Dental School" and "Ideal Charting For General Dentists."
Jeff lectures across the US and now Canada on risk management, recordkeeping and dental ethics.
Jeff founded Lightening Dental Charts, a charting system contains custom progress-note templates, consent forms, Update & Alert bulletins and other legal aids.
Jeff graduated from Indiana University in 1977 and DePaul University Law School in 1981, where he was a member of the law review.
Disclosure(s): No financial relationships to disclose
-
Contains 5 Component(s), Includes Credits
Speaker: Samuel I. Kratchman, D.MD|Endodontic surgery has become a predictable and highly successful way of solving recurrent endodontic infections. Even with the technologies such as operating microscope, CBCT, piezotome, ultrasonics, etc, still there are many situations that arise that require special approaches. This presentation will focus on achieving access to difficult areas, such as palatal roots, or areas covered by thick cortical bone. We will also discuss safe management of the sinuses and mental nerve, as well as a newer concept called selective curettage. When all else fails, then intentional replantation must be considered, and we will discuss techniques to perform replantation with success rates approaching 90%. The presentation is clinically oriented, showing many cases with clinical tips to successful microsurgery.
CE Hours: 2.0
Description: Endodontic surgery has become a predictable and highly successful way of solving recurrent endodontic infections. Even with the technologies such as operating microscope, CBCT, piezotome, ultrasonics, etc, still there are many situations that arise that require special approaches. This presentation will focus on achieving access to difficult areas, such as palatal roots, or areas covered by thick cortical bone. We will also discuss safe management of the sinuses and mental nerve, as well as a newer concept called selective curettage. When all else fails, then intentional replantation must be considered, and we will discuss techniques to perform replantation with success rates approaching 90%. The presentation is clinically oriented, showing many cases with clinical tips to successful microsurgery.
Learning Objectives:
- Demonstrate proper positioning of microscope/patient/doctor
- Troubleshoot potential complications involving the mental nerve and sinuses and palatal roots
- Become comfortable performing Intentional Replantation
Samuel Kratchman, D.MD
CLINICAL ASSOCIATE PROFESSOR OF ENDODONTICS
University of Pennsylvania School of Dental Medicine
Dr. Sam Kratchman was born and raised in New York. He received both a B.S. in Biology and a D.M.D. from Tufts University in Boston. Sam then entered The University of Pennsylvania, where he received a Certificate of Endodontics.
A prominent leader in his field, Dr. Kratchman currently teaches at U. Penn as an Associate Professor of Endodontics, and he is the Assistant Director of Graduate Endodontics, in charge of the microsurgical portion of the program. He frequently lectures on several Endodontic topics throughout the United States, Europe, South America, Canada and Asia.
Dr. Kratchman has authored several articles and chapters on Endodontics, and has co-authored the textbook of Endodontic Microsurgery with Dr. Kim in 2017. He also developed a patented instrument called the S Kondenser for the obturation of root canals. Both Main Line Today and Doctor of Dentistry magazines honored Dr. Kratchman as the cover story for their "Best of" issues.
Disclosure(s): No financial relationships to disclose